Rectal Prolapse – Causes, Symptoms & Advanced Treatment
CM Best Gastro Care & Eye Care | Namakkal
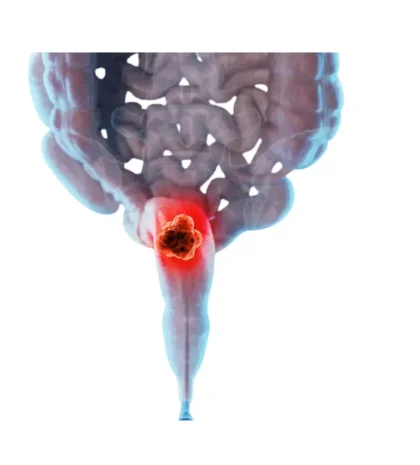
Rectal prolapse occurs when the rectum loses its normal attachments and slides downward, turning itself inside-out and protruding through the anus. Although rarely life-threatening, it causes discomfort, soiling, and progressive pelvic-floor weakness if not corrected promptly.
What Causes Rectal Prolapse?
Chronic constipation or prolonged straining
Weak pelvic-floor or sphincter muscles (age-related or post-childbirth)
Long-standing diarrhea or irritable-bowel disorders
Previous anorectal surgery or neurologic disease
Cystic fibrosis or connective-tissue disorders (in children)
Types of Rectal Prolapse
| Type | Description |
|---|---|
| Mucosal (Partial) | Only the inner rectal lining protrudes. |
| Full-Thickness (External) | Entire wall of the rectum turns outward and is visible. |
| Internal (Intussusception) | Rectum telescopes on itself but does not exit the anus. |
Key Symptoms
A pink or red bulge from the anus, worsening after bowel movements
Mucus discharge, soiling, or dampness in underwear
Feeling of incomplete emptying or rectal pressure
Anal pain, irritation, or minor bleeding
Fecal urgency or leakage (in advanced cases)
Diagnosis
Rectal prolapse is usually confirmed by:
Physical examination while straining.
Proctoscopy / Colonoscopy to exclude tumors or polyps.
Defecography or dynamic MRI to assess internal prolapse.
Anal manometry to measure sphincter strength when continence issues exist.
Treatment Options
1️⃣ Conservative Care (early or partial prolapse)
High-fibre diet & adequate hydration
Stool softeners to avoid straining
Pelvic-floor physiotherapy (Kegel exercises)
Bio-feedback training for sphincter strengthening
2️⃣ Surgical Solutions (full-thickness or persistent cases)
| Procedure | Best for | Highlights |
|---|---|---|
| Laparoscopic Rectopexy | Most adults with good anal tone | Rectum lifted and fixed to sacrum, minimal scars, quick recovery. |
| Laparoscopic Resection Rectopexy | Prolapse + redundant sigmoid colon | Removes excess colon then performs rectopexy. |
| Perineal Delorme Procedure | Frail or elderly patients | Mucosal sleeve excision and muscle plication via anus; low‐risk anesthesia. |
| Perineal Altemeier (Proctosigmoidectomy) | Large prolapse with poor pelvic reserve | Removes distal colon through perineum; may include levator repair. |
Choice of technique depends on age, sphincter strength, comorbidities, and prolapse size.
Post-operative Care & Outlook
Most patients resume light activity within a week after laparoscopic surgery and notice improved bowel control. Lifestyle advice includes fiber-rich meals, pelvic exercises, and avoiding heavy lifting for 6-8 weeks. Early intervention prevents recurrence and protects continence.
Why Choose CM Best Gastro Care?
Advanced laparoscopic & perineal expertise for individualized repair
Comprehensive diagnostics (defecography, manometry) under one roof
Multidisciplinary team for continence rehabilitation and diet counselling
Proven long-term results with low recurrence rates
Dr. Prakashen is widely regarded as one of the best doctors for treating Rectal Prolapse with advanced and minimally invasive gastro care solutions.